
There’s a silent system working round-the-clock to protect women’s reproductive health, and it is not always on the radar. The vaginal microbiome, a colony of mostly beneficial bacteria, is now recognised as one of the most crucial factors in preventing infections and supporting fertility. This ecosystem, though invisible to the eye, plays a massive role in day-to-day health, hormonal balance, and even the success of a pregnancy.
Table of Content:-
For a long time, most of the medical community’s attention was focused on the gut microbiome. But the vaginal microbiome is now stepping into the spotlight, and for good reason. When it’s in balance, it acts like a built-in defence system. When disturbed, it can leave the body vulnerable to repeated infections and even fertility challenges. We spoke to Dr Manjula Anagani, Padmashree Awardee, Clinical Director, Robotic Gynaecologist and HOD, Care Vatsalya, Women and Child Institute, CARE Hospitals, Banjara Hills, Hyderabad, who explained vaginal microbiome health and its impact on your body.
What is the Vaginal Microbiome?
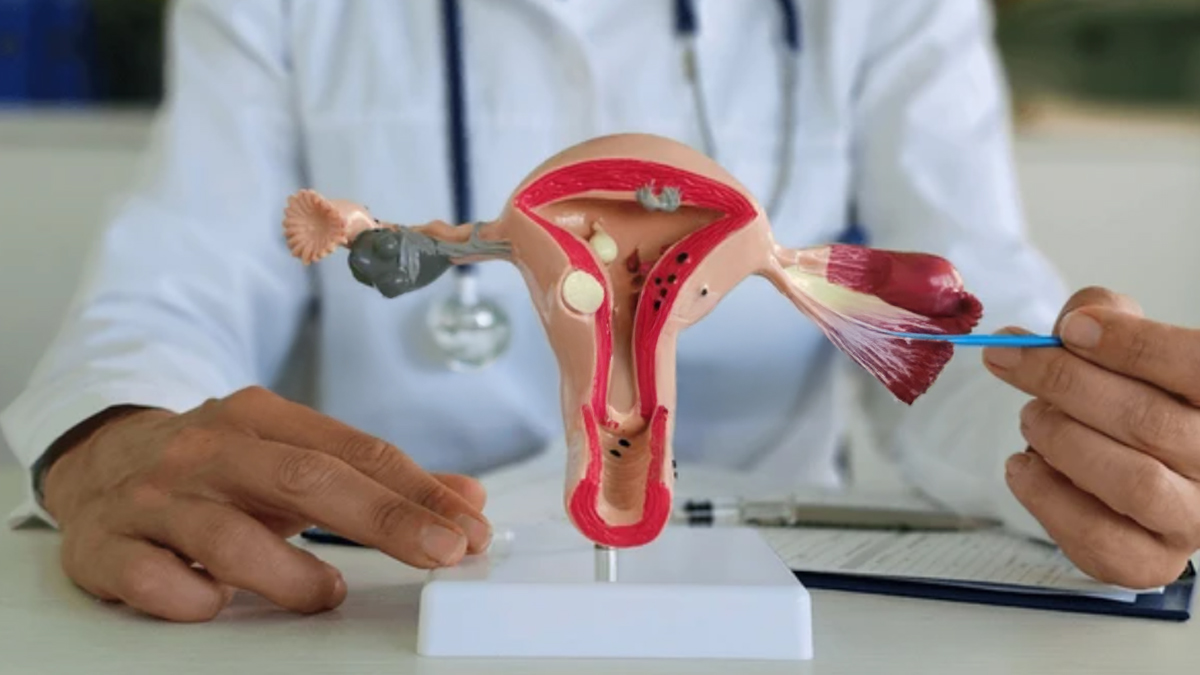
The vaginal microbiome harbours a complex group of microorganisms, most of which are Lactobacillus species. "These lactic acid-producing bacteria maintain the vaginal environment mildly acidic. Acidity is more than a number; it is what suppresses harmful bacteria, yeast, and viruses from thriving," explained Dr Anagani.
Certain species of Lactobacillus also release hydrogen peroxide and other antimicrobial compounds, so the vagina is essentially an independent barrier against infection. "This role becomes vital at important life points, including menstruation, pregnancy, and menopause, when the equilibrium can be easily disturbed," she added.
Why Balance Matters
It takes little to undermine this system. Antibiotics, hormonal fluctuations, stress, poor hygiene, and unprotected sexual contact with new partners can all disrupt the microbial balance. This leads to the emergence of health conditions, such as Bacterial Vaginosis (BV), yeast infections, and urinary tract infections.
“BV, in particular, tends to recur if the microbiome doesn’t bounce back naturally. Although it may seem like a minor issue, BV increases the risk of contracting sexually transmitted infections and has been linked to complications during pregnancy, such as early labour or rupture of membranes,” explained Dr Anagani.
Also Read: 3 Things You Should Do Before Bed As Women To Maintain Your Intimate Health
An Underestimated Role in Fertility

“Reproductive health and microbiome balance go hand in hand. When the vaginal environment is dominated by protective lactobacilli, sperm survival improves, inflammation stays low, and the chances of natural conception go up. On the other hand, a disrupted microbiome can make the vaginal canal more hostile to sperm and less supportive of embryo implantation,” added Dr Anagani.
Women undergoing IVF have shown better success rates when their vaginal and uterine microbiomes are balanced. The presence of certain non-beneficial bacteria has even been associated with early miscarriage or failed implantation. In short, for women trying to conceive, naturally or through assisted methods, the condition of the microbiome cannot be ignored.
According to a 2023 study, in IVF and embryo transfer cases, high abundance of Lactobacillus spp. in both vaginal and uterine microbiomes markedly improves pregnancy rates, while pathogenic bacteria correlate with failed implantation.
During and After Pregnancy
Throughout pregnancy, this microbiome remains a frontline defence. If thrown off balance, it can trigger inflammation that may lead to preterm birth or infections. After delivery, especially in women who breastfeed less or experience hormonal shifts, the microbiome may once again become vulnerable.
In postmenopausal women, falling oestrogen levels affect the thickness of the vaginal lining and the availability of glycogen, which lactobacilli need to thrive. This often results in dryness, discomfort, and an increased risk of infection.
Protecting the Microbiome: What Works?
Simple, persistent habits help to preserve microbial balance:

- Avoid douching or perfumed products: The vagina self-cleans. Excessive use of cleansers or perfumed items can have negative consequences.
- Use antibiotics wisely: If necessary, explore probiotic supplementation during or after treatment.
- Practice safe intimacy: Barrier protection and basic hygiene post-intercourse help reduce bacterial disruption.
- Support through diet: A fibre-rich diet and fermented foods may improve overall microbiota health, including in the vaginal tract. Vaginal or oral lactobacillus probiotics are likely to be beneficial, particularly with recurrent infection or in fertility treatment.
- Address hormonal changes: In women during menopause, local oestrogen therapy is given to restore the mucosal ecosystem, supporting microbiome recovery.
Also Read: Not Just Your Gut Health, Here's How Probiotics Also Help Improve Vaginal Health
A Growing Field in Medicine
Medical science is increasingly recognising that microbiome health is not just a gut issue, it’s a gynaecological priority. “Vaginal microbiome testing is gradually being introduced in fertility clinics, especially for women with unexplained infertility or those with repeated IVF failure. Targeted treatment, including prebiotics, probiotics, and hormone support, is now part of reproductive care in many advanced settings,” said Dr Anagani.
This shift in focus is not only improving fertility outcomes but also reducing the recurrence of infections and improving the quality of life for many women. It’s a reminder that modern gynaecology is moving beyond surface-level symptom management to root-cause approaches.
Bottomline
Dr Anagani concluded, “The vaginal microbiome isn’t just a background player; it’s a key partner in reproductive health. When supported, it reduces the risk of infections, improves fertility, and protects against pregnancy complications. When disrupted, it may silently contribute to a cycle of discomfort, inflammation, and even treatment failure.”
In clinical practice, it's increasingly evident that optimal results occur when the internal ecosystems of the body are honoured and upheld. For women with ongoing infections, difficulties conceiving, or inexplicable discomfort, testing of the microbiome can provide insightful explanations and more effective solutions.
[Disclaimer: This article contains information provided by an expert and is for informational purposes only. Hence, we advise you to consult your professional if you are dealing with any health issue to avoid complications.]
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version
