
The global rise in diabetes is a major concern. Asia, home to 60% of the world's diabetic population, with 65 million in India, faces a significant challenge. Diabetic foot ulcers (DFUs), common in long-term diabetic patients, are hard to heal and can lead to limb amputation. Diabetes is the leading cause of lower limb amputations, with 15-20% of diabetics affected. Treating DFUs consumes 25-50% of diabetes treatment costs. Complications like peripheral arterial disease, neuropathy, foot deformities, and infections contribute to delayed healing.
Table of Content:-
In an Interaction with OnlyMyHealth, Dr (Lt. Col) Pawan K Gupta, President – Medical & Regulatory Affairs at Stempeutics Research, explained about stem cell therapy for diabetic foot ulcers and it’s treatment,
“Despite progress in diabetes control, there's no disease-modifying treatment. Researchers are exploring options to cure DFUs and related complications. Stem cell-based therapies hold promise for intervening in the disease's progression and potentially offering a cure for DFUs,” said Dr Gupta.
Comprehending Diabetic Foot Ulcers
One of the primary causes of chronic diabetic wounds is a flawed wound healing process. In normal wound healing, there is a carefully coordinated interplay involving the formation of connective tissue, cellular activity, and the activation of growth factors. When these physiological processes are disrupted, it leads to ulcers that don't heal properly. Recent studies have delved into these physiological changes to better comprehend the abnormalities in wound healing seen in diabetes.
a) decreased secretion of collagen resulting in chronic connective tissue complications and delayed wound healing,
b) impaired cellular activity due to hyperglycemia resulting in the transformation of macrophages and decreased proliferation of keratinocytes
These ulcers frequently start as little wounds, such as cuts or blisters, which can go unnoticed due to neuropathy. They could develop an infection over time and cause severe problems. Over time, they may become infected and lead to serious complications. Up to 25% of diabetics are predicted to get a foot ulcer at some point in their lives, and this group is at much higher risk for having their feet amputated.
The Potential of Stem Cell Therapy
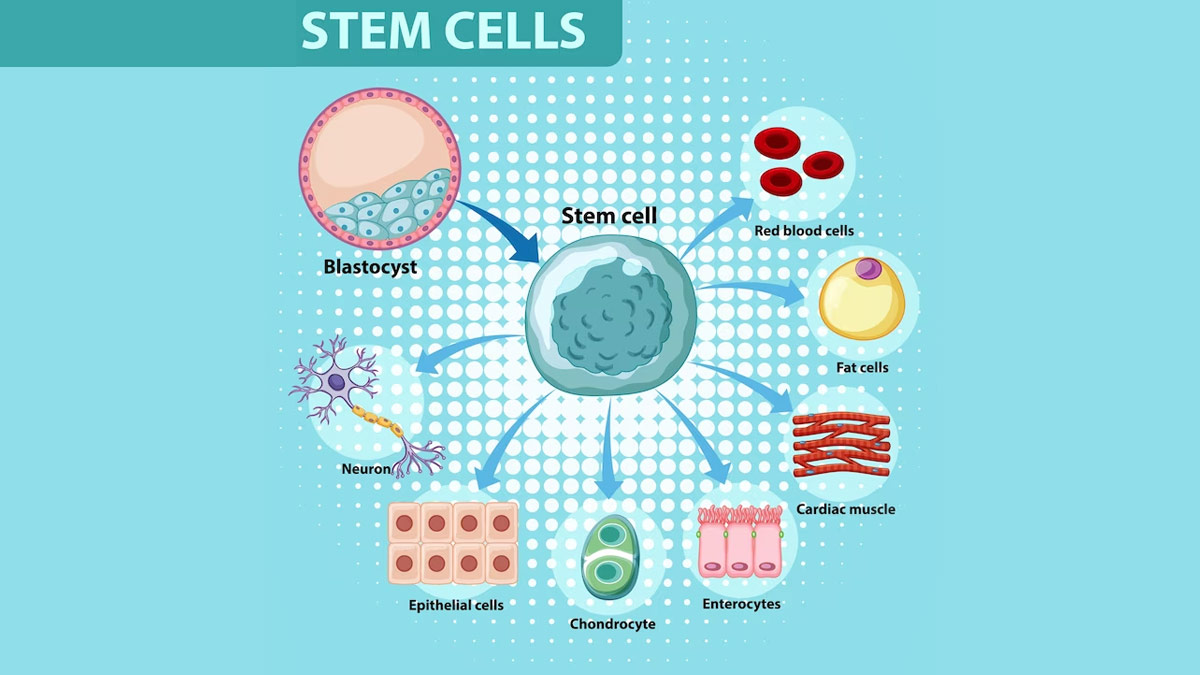
Stem cell therapy, built upon the use of specialised cells capable of transforming into various cell types and aiding in tissue repair, has garnered significant attention in recent years. Its potential to accelerate the healing process of non-responsive diabetic foot ulcers (DFUs) is a key driver of this interest.
Also read: Stem Cell Therapy Can Deal With Kidney Problems, Read Details Inside
Mesenchymal Stromal Cells (MSCs) – potential source for wound healing
MSCs, a type of adult stem cell, are preferred for enhancing skin wound healing in regenerative medicine. They are easy to isolate, scalable, accessible from various tissue sources, and suitable for both self and donor therapies. MSCs are well-suited for wound healing as they interact with and support the body's cells and tissues through multiple interactions. Bone marrow derived MSCs, commonly used, contribute to repairing various degenerating tissues.
Proposed mechanism of action of MSCs for healing diabetic wounds
MSCs aid dermal regeneration across multiple wound healing phases. They exhibit anti-inflammatory properties, dampening the immune response by reducing immune cell activity. MSCs increase prostaglandin E2 (PGE2) production, an anti-inflammatory molecule, altering immune cell behaviour and promoting wound fibroblast activity. This makes them well-suited for inflamed environments.
MSCs secrete cytokines, chemokines, and growth factors that support wound healing. In the proliferative phase, they stimulate tissue and blood vessel growth through factors like VEGF-A, IGF-1, KGF, ANG-1, SDF-1, and PDGF. MSCs enhance macrophage function, reducing inflammation. They also impact wound matrix remodelling, resulting in tissue that closely resembles uninjured areas. Overall, MSCs contribute to scarless tissue formation during wound healing.
Top of Form Clinical Trials and Success Stories
Various stem cell therapies have shown promise in treating diabetic foot ulcers (DFU). Here are key findings from relevant clinical trials:
Jain et al. conducted a prospective study in DFU patients, applying bone marrow-derived cells or whole blood (control) topically and locally. The treatment group (n=25) saw a 17.4% average reduction in wound area at 2 weeks, compared to 4.84% in the control group (n=23). After 12 weeks, the treatment group had a 36.4% average decrease in wound area, while the control group showed a 27.32% reduction. This study indicated that a single application of autologous bone marrow-derived cells accelerated DFU healing, especially in the early treatment stages.

Another study involved intramuscular injection of BM-MSCs, BM-MNCs, or normal saline in 41 type 2 diabetic patients with foot ulcers. After 6 weeks, ulcer healing was significantly higher in the BM-MSC group compared to the BM-MNC group (p = 0.022), and BM-MSC-treated ulcers achieved 100% healing four weeks earlier than BM-MNC-treated ulcers. Moreover, the number of healing ulcers in the BM-MSC group was significantly higher than in the normal saline group 4 weeks after transplantation.
Dash et al. investigated the efficacy of autologous BM-MSCs in treating non-healing ulcers in 24 patients with various underlying causes, including type 2 Diabetes Mellitus and Buerger’s disease. In the diabetic foot ulcer group, ulcer size decreased significantly from 7.26 ± 1.41 cm2 to 2 ± 0.98 cm2 (p < 0.001) at the 12-week follow-up. The study concluded that BM-MSCs accelerated the healing of non-healing ulcers of different disease origins.\
Also read: Stem Cell Therapy for Hair Growth
Moreover, several anecdotal success stories underscore the potential of stem cell therapy in treating diabetic foot ulcers (DFU). Patients with previously non-healing ulcers, which had prompted consideration of amputation, have experienced significant improvements and, in some cases, complete healing following stem cell therapy.
Wound healing involves ECM, growth factors, and cells, with MSCs playing a pivotal role in all phases: inflammation, proliferation, and remodelling. They control inflammation, aid in wound clearance, and promote transition to proliferation. MSCs release growth factors for granulation and epithelialisation and facilitate organised ECM deposition in remodelling.
Few wound treatments harness MSC benefits, especially for challenging wounds. Efforts to develop innovative bioengineered products are ongoing, recognizing MSCs' role.
To make stem cell therapies commonplace for diabetic foot ulcers (DFUs), collaboration between experts, researchers, and regulators is essential. Despite obstacles, stem cell therapy offers hope in the fight against this debilitating diabetes complication, improving DFU patient outcomes.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version