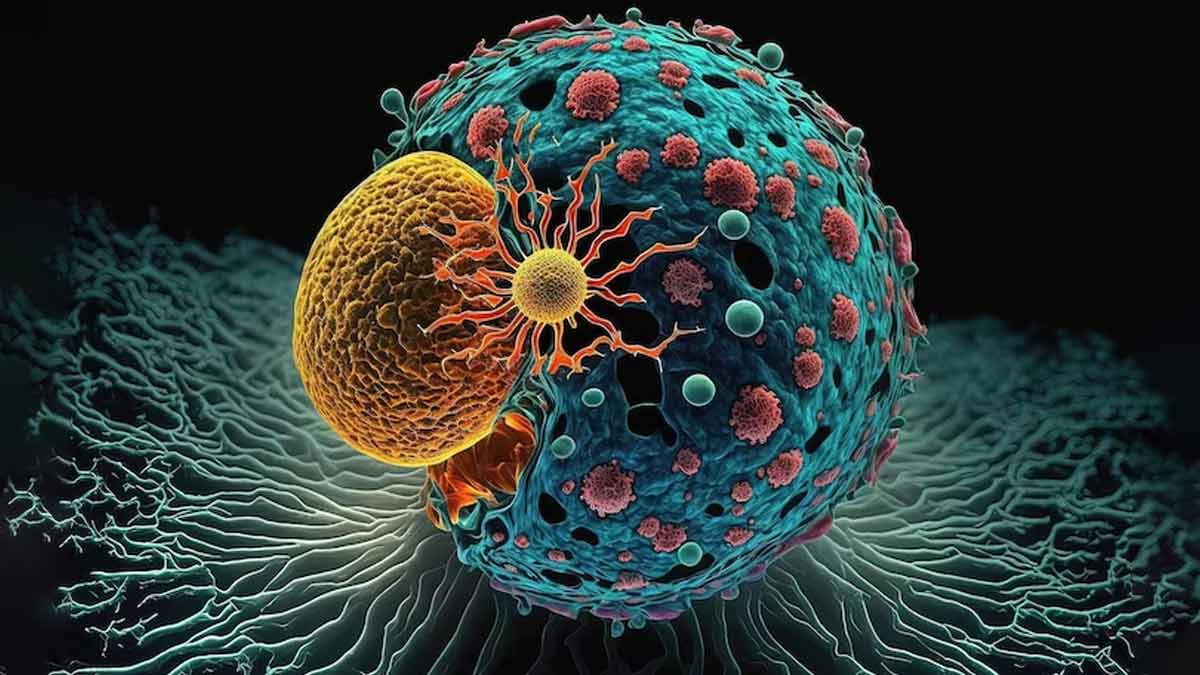
In the realm of cancer care, every breakthrough represents a glimmer of hope. And the field of oncology has witnessed a revolutionary advancement in cancer treatment with the emergence of CAR -T Cell therapy. This groundbreaking approach represents a new frontier in cancer care, offering hope to patients with certain types of cancer that were previously considered untreatable. As the medical community continues to unravel the complexities of CAR-T cell therapy and its implications for cancer treatment, it is crucial for both healthcare professionals and patients to gain a deeper understanding of this transformative technology. In an interaction with Only My Health, Dr Nataraj K S - Sr Consultant, Hemato Oncology & Transplant Physician, HCG Cancer Center, KR Road, Bangalore, explained all about CAR-T cell therapy.
Table of Content:-
What is CAR- T Cell therapy?
“CAR-T cell therapy, short for chimeric antigen receptor T cell therapy, is a type of immunotherapy that harnesses your body’s immune system to fight cancer cells more effectively. It involves modifying a patient's T-cells (a type of immune cell) to express a specific receptor, known as a chimeric antigen receptor (CAR), enabling these cells to target and kill cancer cells,” said Dr Nataraj. “It holds immense promise for patients with blood cancers who have had other standard treatments, like chemo or transplant, but the cancer came back or didn’t get better. Right now, CAR T cells are not an option for people who have been newly diagnosed with blood cancer,” Dr added.

Understanding the Treatment
Collection of T cells from a patient: Apheresis is a procedure that removes blood components (such as plasma, platelets, and white blood cells) from the body so that T cells can be collected. The remaining blood is then returned to the body.
T cells are reengineered in a laboratory: To make chimeric antigen receptors (CARs), the T cells are genetically engineered in a lab or a drug manufacturing facility by introducing DNA into them. CARs are proteins that allow the T cells to recognize an antigen on targeted tumour cells.
Also read: Smoking And Cervical Cancer: Expert Explains The Link And Why Quitting Matters
Multiplying the re-engineered CAR T cells: After being expanded in the lab, the genetically modified T cells are frozen for 3 to 4 weeks before being sent to the patient's treatment facility.
Infusing the CAR T cells into the patient. Many patients undergo the process of lymphodepletion (brief course of one or more chemotherapy drugs to reduce the number of normal t cells) before they receive the infusion of CAR T cells to make space for the new CAR T cells. This is followed by a less than 30-minute IV infusion of the new CAR T cells, which multiply in the bloodstream to target and eliminate antigen-presenting cells.
Guarding against recurrence. Not only CAR T cells can eradicate all cancer cells in the body, but they may remain in the body months after the infusion. The therapy has resulted in long-term remissions for some patients with certain types of blood cancer.

Benefits of car-t cell therapy?
Despite being a relatively new form of treatment, CAR-T cell therapy has shown promising benefits, especially for patients with blood cancers who no longer respond to other treatment forms.
1.Revitalising Patients with Refractory or Relapsing Conditions
Unlike chemotherapy, CAR-T cell therapy has achieved spectacular remission rates in people with relapsed or refractory acute lymphoblastic leukaemia (ALL) or non-Hodgkin lymphoma (NHL).
Also read: Oesophageal Cancer: Innovations In Surgical Techniques for better treatment
2.Long-Term Remission
There is evidence that CAR-T therapy offers durable remissions for many patients - that is, the cancer remains at bay for a prolonged period after treatment. This spares patients from the continuous cycle of cancer treatments while simultaneously enhancing their quality of life.
3.Highly Personalised Treatment
Unlike standard cancer therapies, CAR-T cell treatment is highly individualised. The T-cells used for therapy are collected from the patient, modified, and then reintroduced, increasing the likelihood of a positive outcome and making treatment safer for the patient as a whole.
The development of CAR-T cells represents a milestone in the ongoing fight against cancer, as it offers hope to patients who have previously been unable to receive treatment. With cancer treatment entering a new era, let's remain committed to pushing the limits of what is possible, guided by the belief that every patient deserves a fighting chance.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version