
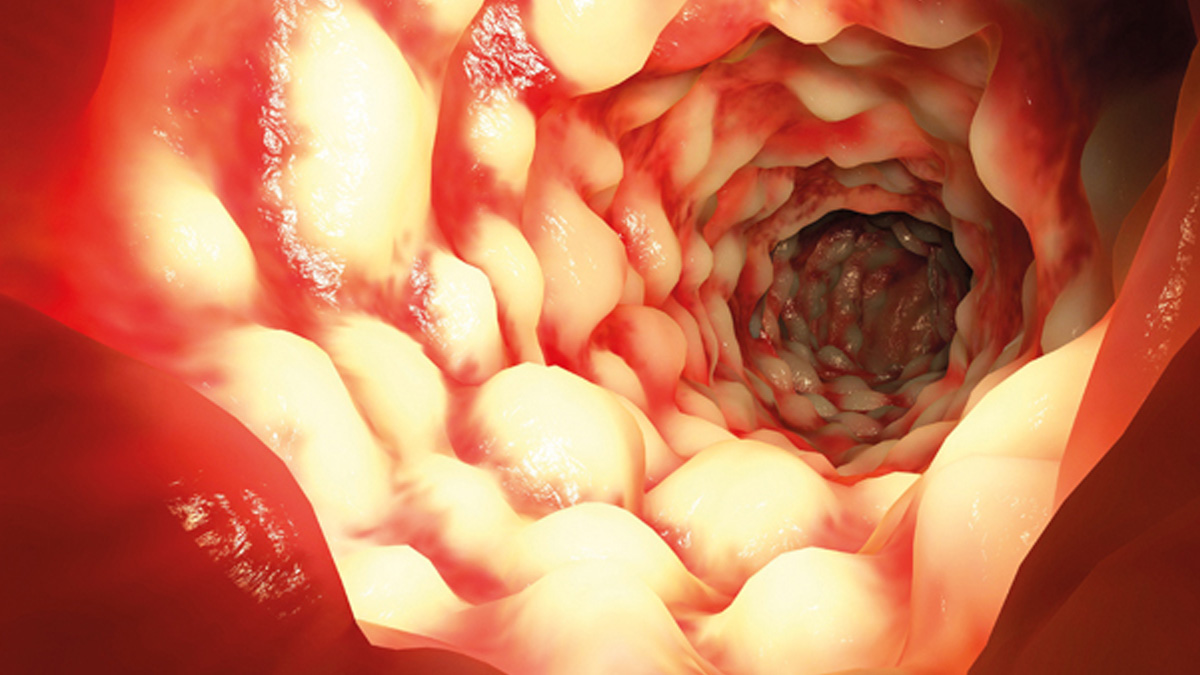
Colorectal cancer, commonly known as bowel cancer, is a significant concern for individuals diagnosed with inflammatory bowel disease (IBD), which includes conditions such as ulcerative colitis and Crohn’s disease. Due to chronic inflammation in the intestinal lining, people with IBD have a heightened risk of developing abnormal cell growth, known as dysplasia, which can lead to cancer. Traditionally, routine colonoscopies have been the primary method for detecting early signs of cancer in these patients. However, a groundbreaking new test may revolutionize how colorectal cancer risk is predicted in individuals with IBD.
Table of Content:-
The Link Between IBD and Colorectal Cancer
Research has long established that chronic inflammation associated with IBD creates an environment conducive to the development of precancerous polyps in the colon. Over time, these polyps can progress into colorectal cancer. Current guidelines recommend that people with IBD undergo routine colonoscopies every one to three years to monitor for early signs of cancer. Despite these preventive efforts, identifying precancerous changes through colonoscopy remains challenging.

Scientists have been searching for a more precise method to determine which IBD patients are at the greatest risk of developing colorectal cancer. Researchers from The Institute of Cancer Research in London may have found the answer. They have developed a test capable of predicting bowel cancer risk with over 90% accuracy, marking a significant advancement in early cancer detection.
Also Read: Donald Trump Halts USAID—What It Means for India’s Healthcare Sector
A Genetic Approach to Predicting Cancer Risk
The new test, developed by a team led by Dr Trevor Graham, professor of genomics and evolution, offers a more refined way of assessing cancer risk in people with IBD. According to Dr. Graham, the inability to accurately predict which patients will develop cancer has led to a difficult dilemma—some patients undergo life-altering surgeries to remove sections of the colon as a precaution, while others live with uncertainty about their cancer risk.
To address this issue, researchers examined the genetic composition of precancerous cells in IBD patients. They discovered that those who exhibited significant DNA changes—such as multiple copies of DNA being gained or lost—were at an elevated risk of developing colorectal cancer. This finding led to the development of an algorithm that assesses the genetic profile of a patient's biopsy sample to determine their likelihood of developing cancer in the future.
Over 90% Accuracy in Predicting Colorectal Cancer
The effectiveness of this test is remarkable. In the study, researchers found that the test could accurately predict which patients with precancerous changes would go on to develop colorectal cancer within five years—with an accuracy rate exceeding 90%.

Dr. Graham emphasized that the test could be life-changing for IBD patients. Those identified as high risk could opt for surgery to eliminate their cancer risk, while those with a low risk could avoid unnecessary invasive procedures and alleviate anxiety. However, before the test can be widely adopted, further clinical trials are needed to confirm its effectiveness in real-world settings.
A Step Toward Less Invasive Monitoring
Medical experts have welcomed this development, noting that it could significantly reduce the need for frequent colonoscopies in IBD patients. Dr. Rudolph Bedford, a gastroenterologist at Providence Saint John’s Health Center in Santa Monica, praised the test as a game-changer. He explained that frequent colonoscopies and biopsies are currently the norm for IBD patients, which can be both physically uncomfortable and emotionally stressful.
With a test that offers highly accurate predictions, medical professionals could target their treatments more effectively, reducing the need for repeated invasive procedures. This would not only improve patient care but also provide greater clarity and peace of mind for those managing IBD.
Bottomline
This breakthrough test represents a significant leap forward in personalized medicine. By utilizing genetic markers to determine cancer risk, it paves the way for more tailored treatment approaches. If clinical trials continue to support the test’s accuracy, it could soon become a standard tool in managing colorectal cancer risk for IBD patients. For now, the findings offer hope that more precise and less invasive cancer risk assessments are on the horizon, ensuring that treatment is targeted where it is needed most.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version