In February 2025, Ryan Alto, a 48-year-old from California, developed what seemed like a routine flu. He had a headache, body aches, and general fatigue, but within hours of driving himself to the hospital, his condition spiralled. He began hallucinating, had seizures, and slipped into a coma that lasted eight weeks. The diagnosis? A rare neurological condition called anti-NMDA receptor encephalitis.
Table of Content:-
Months later, Ryan was still unable to walk or fully recognise the world around him. His family described his recovery as slow and painful, with frequent confusion and fragile cognition.
His story is not an isolated one. Many people, especially young women, present with similar symptoms, which are often mistaken for mental health issues or a viral infection.
Also Read: Rainy Season Alert: The Hidden Dangers Of Brain-Eating Amoeba In Pools And Tanks
What Is Anti-NMDA Receptor Encephalitis?

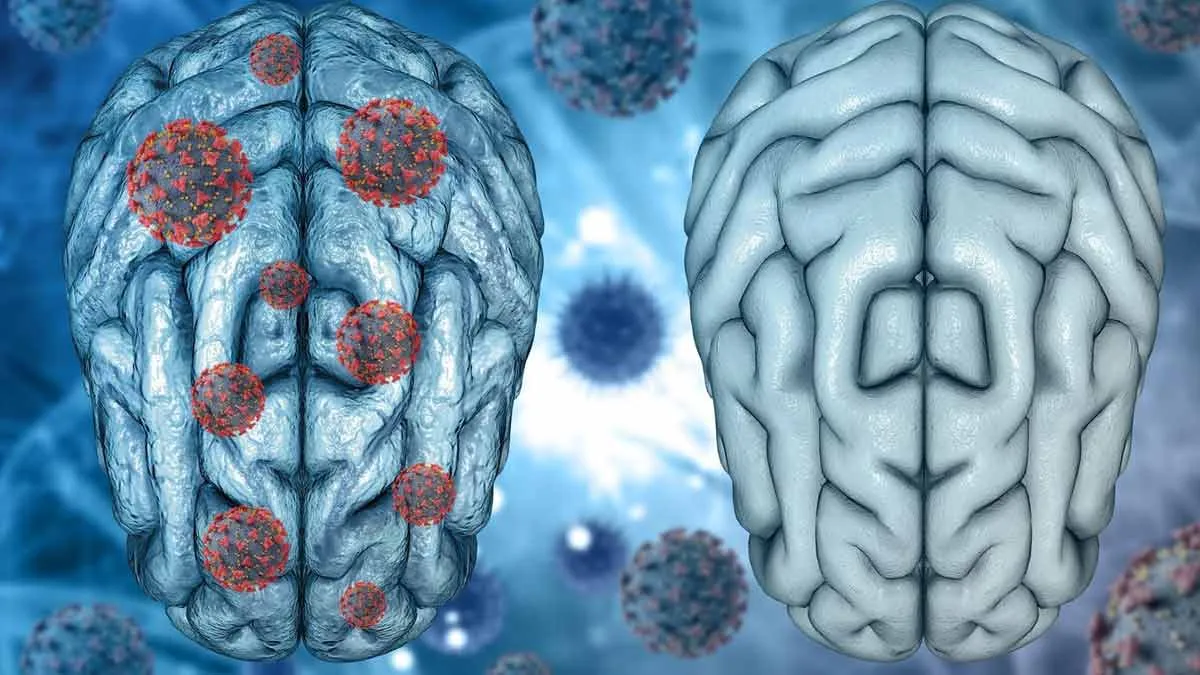
According to Dr Rahul Chakor, Consultant Neurologist, Jaslok Hospital & Research Centre, Mumbai, "Anti-NMDA receptor encephalitis is an autoimmune neurological disorder, in which the body’s immune system produces antibodies against the NMDA (N-methyl-D-aspartate) receptors in the nervous system."
The disease affects the brain’s limbic system, which regulates emotion and behaviour. What begins as tiredness or fever can soon lead to severe psychiatric and neurological symptoms, including agitation, paranoia, confusion, seizures, and coma.
According to StatPearls Publishing, anti-NMDAR encephalitis is a rare disease, which affects one out of 10.5 lakh people per year. However, it is the best known and probably the most common autoimmune encephalitis.
Why Early Symptoms Are Often Misdiagnosed

In its early stages, the condition can look deceptively mild. “Initial symptoms are non-specific and include fever, headache, fatigue, and malaise, general feeling of being unwell,” says Dr Chakor. Within days to weeks, people may develop severe anxiety, agitation, or hallucinations, leading to misdiagnosis as schizophrenia or psychosis.
This overlap means that many patients, especially women, are first admitted to psychiatric facilities rather than neurology wards, delaying critical treatment.
Causes Behind This Autoimmune Attack
One common cause is paraneoplastic syndrome, where a tumour, often an ovarian teratoma in young women, triggers the immune system to create antibodies that also target the brain.
“Infections like herpes simplex virus can also lead to molecular mimicry,” Dr Chakor adds, where the immune system gets confused and attacks healthy brain tissue. This can happen even weeks after a viral infection has cleared up.
How Is Anti-NMDA Receptor Encephalitis Diagnosed?

Anti-NMDA receptor encephalitis is diagnosed through a combination of clinical tests. Doctors may order an MRI, EEG (to detect brain activity irregularities), and a lumbar puncture (spinal tap) to look for anti-NMDA antibodies in cerebrospinal fluid.
In young women, a pelvic ultrasound or PET scan may be used to check for ovarian teratomas or other hidden tumours.
Treatment And Chances Of Recovery
Treatment involves calming the immune system and removing the source of the antibody attack, if one is found. This includes immunotherapy (such as steroids or IVIG), plasmapheresis (a process to filter harmful antibodies from the blood), and surgery to remove any tumour.
Patients may also need antipsychotic medication, anti-seizure drugs, and extensive rehabilitation. Some patients regain full cognitive function within months; others may need ongoing therapy and support for years.
Why Awareness Is Crucial
Anti-NMDA receptor encephalitis is still under-recognised. Because its early signs mimic common infections or psychiatric conditions, many patients suffer delays in getting the right diagnosis and treatment. Greater awareness, among both the public and medical professionals, can lead to earlier intervention and better outcomes.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version