Imagine a child who keeps falling sick, looks pale, and has a swollen belly. The parents visit many doctors but find no answers. Finally, after months of worry, the child is diagnosed with a lysosomal storage disorder, a rare, serious illness most people have never heard of. It is deadly if not treated and is becoming more common in India. Sadly, because it is so rare, many families don’t know about it or how dangerous it can be until it’s too late. Early diagnosis and treatment can change lives, but awareness is still very low.
Table of Content:-
Understanding Lysosomal Storage Disorders![Lysosomal Storage Disorders 3 - 2025-06-18T164921.462]()
Dr Priyanshu Mathur, Professor, Department of Medical Genetics, SMS Medical College, Jaipur, explains, “Lysosomal Storage Disorders are a rare inherited disorder where a fatty substance called glucocerebroside builds up in the body. This happens because the body is missing an important enzyme, called glucocerebroside, needed to break down this fat.” This buildup mainly affects the liver, spleen, bone marrow, and sometimes the brain. Over time, these organs stop working properly, leading to many health problems.
Under India’s National Policy for Rare Diseases (NPRD) 2021, Lysosomal Storage Disorders (LSDs) are primarily categorised under Group 3 (a). Below is the detailed breakdown of all rare diseases categorised under NPRD 2021:
- Group 1: amenable to one-time curative treatment,
- Group 2: long-term/lifelong treatment having relatively lower cost of treatment with special dietary, and hormone therapy, etc., and benefit has been documented in literature, and annual or more frequent surveillance is required
- Group 3 (a): Diseases for which definitive treatment is available & sufficient evidence for good long-term outcomes exists, such as Enzyme Replacement Therapy for Gaucher, MPS I & II, Fabry, Pompe, known as Lysosomal Storage Disorders)
- Group 3 (b): For these disorders, the cost of treatment is very high and long-term follow-up literature is awaited or has been done on a small number of patients.
What Causes Lysosomal Storage Disorders?![gaucher disease 1 - 2025-06-18T164923.522]()
All LSDs share a genetic cause: mutations in genes that code for lysosomal enzymes or transporters. These mutations hinder the breakdown of substrates, causing them to build up in cells.
For example:
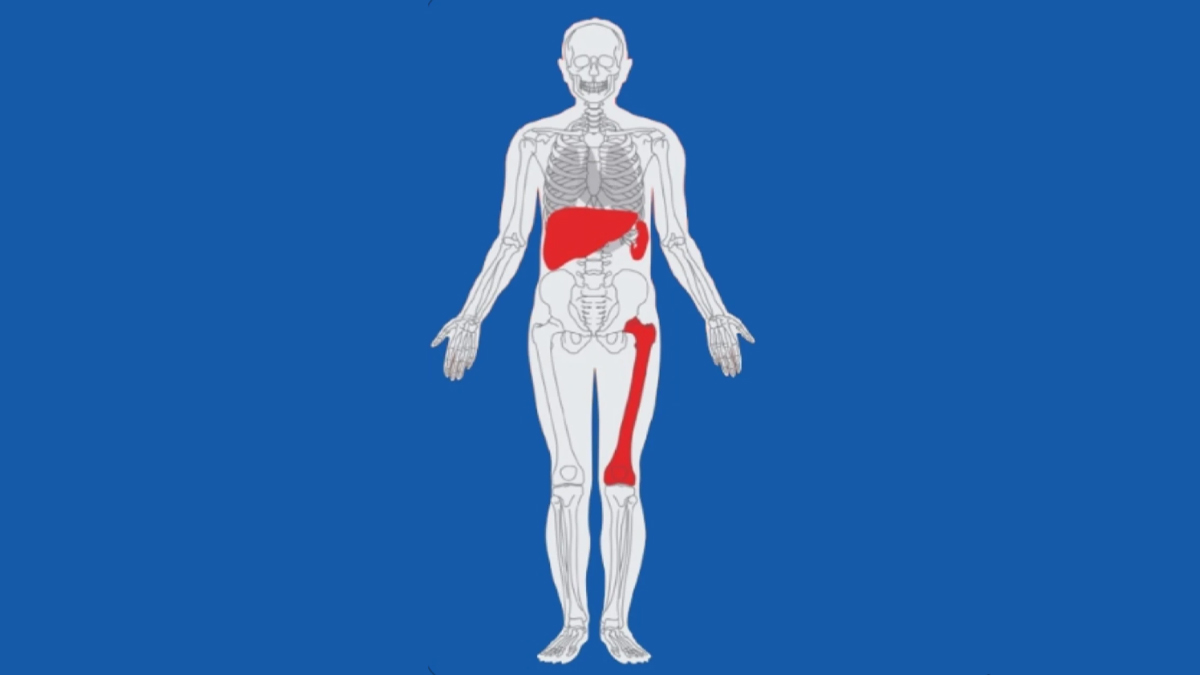
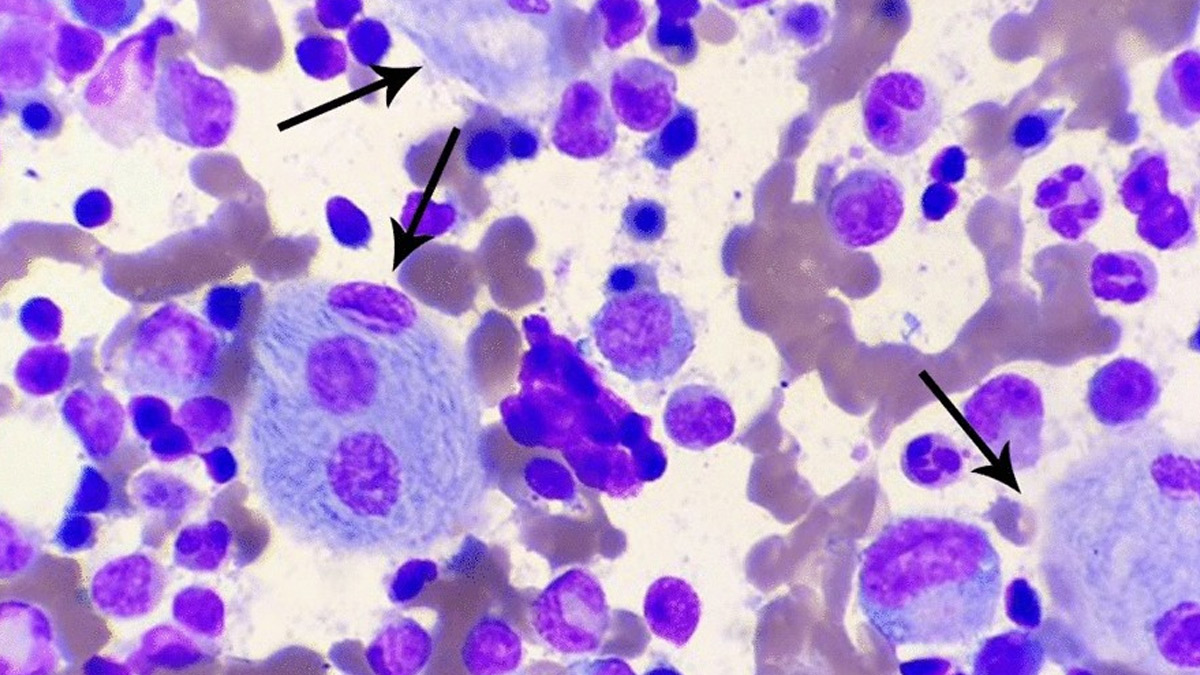
- Gaucher disease: Gaucher disease is caused by a change (mutation) in the GBA gene. Dr Mathur explains that this gene tells the body how to make the enzyme glucocerebrosidase. Without enough of this enzyme, the fatty substance glucocerebroside cannot be broken down. Instead, it collects inside certain white blood cells called macrophages. These cells then turn into “Gaucher cells,” which spread and damage organs.
- Mucopolysaccharidoses (MPS): Mucopolysaccharidoses (MPS) are among the group of inherited ultra-rare Lysosomal Storage Disorders (LSDs) caused by the absence or malfunctioning of specific enzymes required to break down glycosaminoglycans (GAGs). These complex sugars, when not broken down, accumulate in cells and tissues, causing progressive and multi-system damage.
Complications Associated With LSDs
Depending on the specific disorder, LSDs can manifest with a range of serious complications:
- Organomegaly and haematological issues: e.g., Gaucher–associated liver and spleen enlargement, anaemia, thrombocytopenia
- Skeletal problems: due to substrate deposition in bones and cartilage (common in Gaucher and MPS)
- Neurological decline: especially in LSDs with CNS involvement (e.g., neuronopathic Gaucher)
- Cardiac and renal issues: For conditions like Fabry disease, substrate buildup can harm vessels, kidneys, and the heart.
Treatment Options for LSDs![Lysosomal Storage Disorders treatment 4 (62)]()
According to Dr Mathur, the treatment of the disease is challenging but possible. Enzyme Replacement Therapy (ERT) has changed the lives of many people with Lysosomal Storage Disorders (LSDs) like Gaucher, MPS, Fabry, and Pompe diseases. ERT works by giving patients the missing enzyme their bodies need. This helps lower the build-up of harmful substances in their cells. As a result, patients often see smaller liver and spleen sizes, better breathing and heart function, more energy, and improved growth in children.
- Disease-Specific Factors: The effects of discontinuing ERT vary greatly depending on the specific disease and the individual’s response to therapy. Some patients may tolerate interruptions better than others, but for most LSDs, continued treatment is crucial to prevent disease progression.
- Timing of Reinitiation: The earlier therapy is restarted, the better the chances for partial recovery or stabilisation. However, delays in reinitiating ERT can lead to irreversible damage, particularly in the nervous system.
- The introduction of ERT significantly modified the natural course of the disease, notably slowing disease progression and mitigating the severity of symptoms.
Challenges in Treating Lysosomal Storage Disorders in India
Dr Mathur highlights that the treatment is very expensive. ERT can cost between ₹40 lakh and ₹1 crore per year, depending on the patient’s weight. Also, you need lifelong therapy and regular hospital visits. There are very few specialised centres in India, and many doctors are not aware of the disease. The expert lists what makes the treatment difficult:
- High cost and lifelong therapy required
- Limited availability of specialised centres for enzyme infusions
- Delayed diagnosis due to a lack of awareness
- Challenges in managing neurological symptoms in Types 2 and 3
- Treatment doesn’t reverse damage already done to bones or the brain
Without treatment, lysosomal storage disorders can become life-threatening. The liver and spleen can grow so large that they need to be removed. Severe anaemia, infections, and bone problems can lead to disability. In the severe types, children can have seizures, lose their vision, and die very young. Growth is stunted, and quality of life is poor.
Conclusion
With early and regular treatment, many complications can be prevented. Children can go to school, play, and grow normally. Adults can work and live almost normal lives. Early treatment turns a deadly disease into a manageable one. Gaucher disease is a rare but deadly illness that is often missed or misunderstood, especially in India. It affects children and adults, causing serious health problems if not treated. With early diagnosis and the right treatment, patients can live better, healthier lives. Raising awareness and improving access to treatment can save lives and give hope to many families.
Also watch this video
Read Next
Is Your Liver in Trouble at Night? Doctor Explains Red Flags of Fatty Liver You Shouldn’t Ignore
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version
-1750246086834.jpg)