
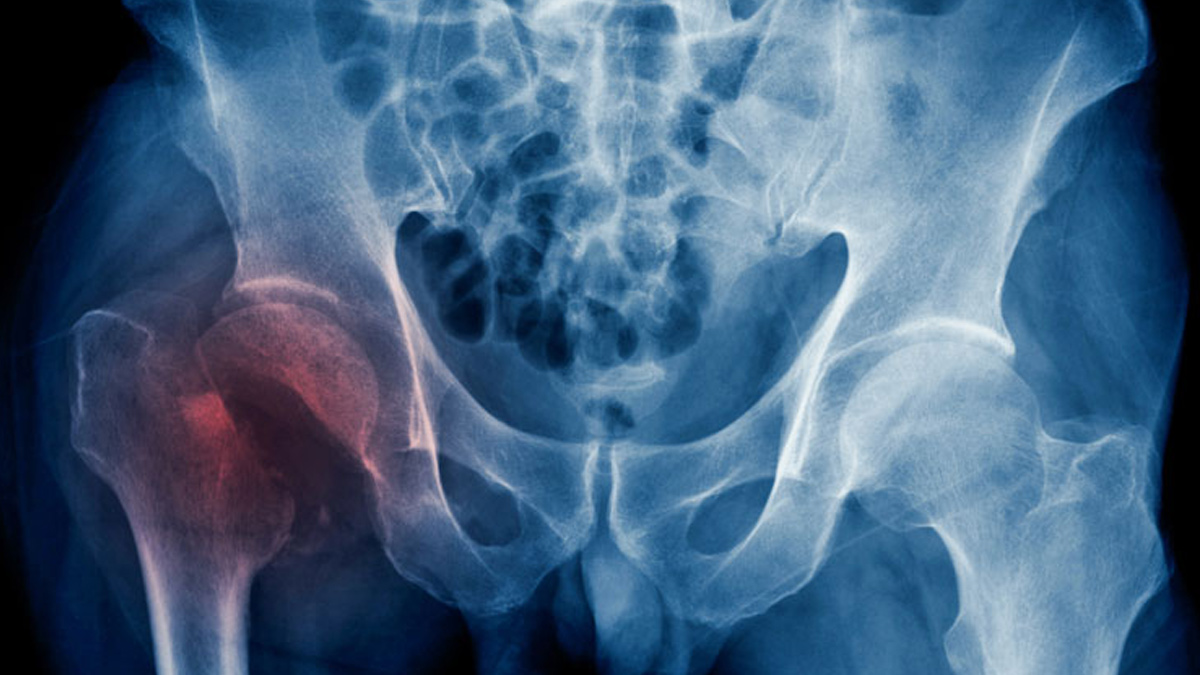
Type 2 diabetes has long been associated with various health complications, but recent research highlights a significant concern for older women: an increased risk of fractures. Contrary to earlier beliefs that suggested lower bone density might be responsible, new findings indicate that the real issue lies in the overall physical health and functional capabilities of these individuals.
Table of Content:-
Understanding the Link Between Type 2 Diabetes and Fractures
Historically, studies on bone density in individuals with type 2 diabetes have yielded mixed results. Some research suggested that bone density in people with diabetes might be higher than average, while others noted that bone structure could be compromised, making bones more susceptible to fractures despite seemingly normal or increased density. A recent study conducted by Swedish researchers provides a clearer picture of why older women with type 2 diabetes face a higher fracture risk.
The Study: Key Findings and Methodology
Researchers from Gothenburg University and Sahlgrenska University Hospital analyzed data from 294 women with type 2 diabetes and 2,714 women without diabetes, all aged 75 to 80. The data was sourced from the Sahlgrenska University Hospital Prospective Evaluation of Risk of Bone Fractures study cohort, which includes comprehensive information on participants' medical histories, physical activities, and bone health.
Key findings from the study revealed that while women with type 2 diabetes had marginally higher bone density, their physical function was significantly impaired compared to their non-diabetic counterparts. This was evident in several areas:
- Bone Density: Women with diabetes showed a 4.4% higher bone density in the hip and similar increases in other areas like the femoral neck and lumbar spine. However, there was a slight decrease in density in other parts of the spine.
- Physical Function: Participants with diabetes scored 19.2% lower on the Physical Activity Scale for the Elderly. They also performed poorly in balance tests and other physical activities, such as standing on one leg and rising from a chair.
These findings suggest that while bone density might be slightly higher in diabetic women, their reduced physical ability and balance are more critical factors contributing to their increased fracture risk.
Also Read: Cancer Cases And Deaths In Men Predicted To Increase By 93% By 2050: Study
Implications of Physical Function on Fracture Risk
The study underscores that the increased fracture risk among older women with type 2 diabetes is not due to lower bone density but rather due to diminished physical function. Poor balance, slower movement, and lower strength increase the likelihood of falls, which are a primary cause of fractures in this population. Dr. Mattias Lorentzon, the study’s lead author, emphasized that the poor physical function observed in diabetic women, rather than any difference in bone characteristics, is the main reason for their heightened fracture risk.
Impact of Diabetes Medications on Bone Health
The research also explored the effects of diabetes medications on bone health. Women taking insulin had a 71% higher risk of fractures, while those on oral diabetes medications faced a 27% increased risk. Interestingly, while these medications were associated with higher bone density and better bone microarchitecture, they were also linked to poorer physical performance. This highlights a complex relationship between diabetes treatment, bone health, and physical function.
Understanding the Mechanisms: Diabetes and Bone Health
Dr. Yoshua Quinones, an internist who reviewed the study, explained that despite having denser bones, individuals with type 2 diabetes experience a higher fracture risk due to poorer bone quality. Factors such as elevated blood sugar levels and chronic inflammation can damage bone tissue and compromise bone strength. Additionally, diabetes can impair balance and vision, further increasing the risk of falls.
Future Directions and Recommendations
Given the findings, there is a clear need to address physical health in managing fracture risk among older women with type 2 diabetes. Improving physical function through targeted interventions, such as strength training and balance exercises, could potentially reduce the incidence of falls and fractures in this vulnerable population.
Also Read: HIIT May Be More Effective Than Moderate Exercise After A Stroke: Study
Dr. Lorentzon's team plans to investigate whether enhancing physical function can indeed lower fracture risk for people with diabetes. This approach could offer a practical solution to mitigating one of the significant health challenges faced by older adults with type 2 diabetes.
Bottomline
The recent study sheds light on the complex relationship between type 2 diabetes, bone health, and fracture risk. While bone density might be slightly higher in individuals with diabetes, it is their overall physical health and functional limitations that significantly contribute to their increased risk of fractures. Addressing these physical impairments could be crucial in reducing fracture risks and improving the quality of life for older women with type 2 diabetes.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version
