
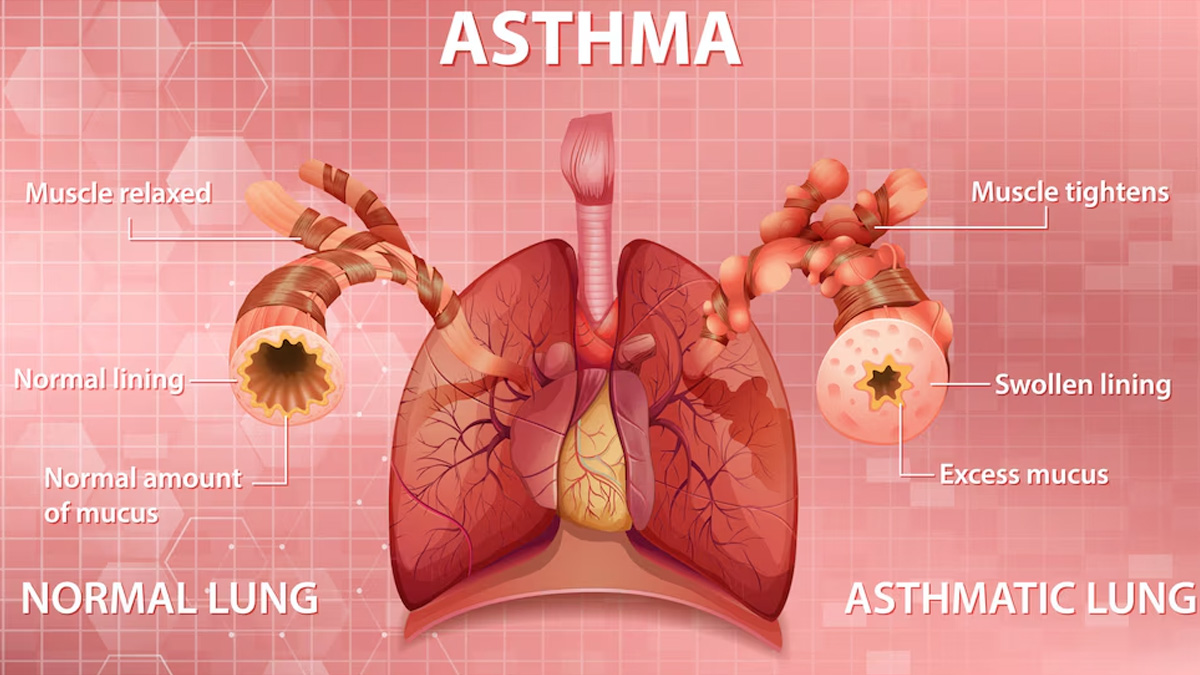
Asthma is a chronic respiratory disease affecting over 300 million people worldwide. Characterised by airway inflammation and hyperresponsiveness, it can lead to symptoms such as breathlessness, coughing, and wheezing. While environmental triggers like allergens and pollution are well-known contributors, recent research highlights the crucial role of immune cells in the development and severity of asthma.
Table of Content:-
The Role of Immune Cells in Asthma
To understand the role of immune cells in asthma, OnlyMyHealth team spoke to Dr N Sai Samhita, MBBS, General Physician and Telemedicine Consultant, Hyderabad. According to her, asthma is heavily influenced by immune cell activity.
"Asthma is a chronic respiratory condition marked by airway inflammation and hyperresponsiveness, significantly impacting the lives of over 300 million people globally," she said.
A variety of immune cells are involved in the inflammatory response that defines asthma, particularly in individuals with a "Type-2-high" phenotype. Dr Samhita says that this subset of asthma patients exhibits heightened immune activity, driven by specific cells, including:
T helper type 2 (Th2) cells – These play a pivotal role in asthma inflammation by releasing cytokines like IL-4, IL-5, and IL-13, which contribute to airway hypersensitivity and mucus production.
Innate lymphoid cells type 2 (ILC2s) – These cells amplify type 2 inflammation by responding to allergens and producing similar cytokines to Th2 cells.
- Eosinophils – These white blood cells accumulate in the airways, exacerbating inflammation and tissue damage.
- Mast cells – When activated by allergens, they release histamines and other inflammatory mediators that contribute to asthma symptoms.
- Regulatory T and B cells – These cells play a balancing role in immune responses, but dysfunction in their regulation can lead to uncontrolled inflammation.
"Recent research highlights the critical role of various immune cells in the pathogenesis of asthma, particularly T helper type 2 (Th2) cells, innate lymphoid cells type 2 (ILC2s), eosinophils, mast cells, and regulatory T and B cells," says Dr Samhita.
Also read: Why Does Winter Worsen Asthma Symptoms? Doctor Shares Tips To Combat
The Controversy Around Immune-Based Asthma Treatments
Asthma treatment has evolved significantly with the introduction of biologic therapies that target specific immune cells and cytokines. However, their efficacy remains a topic of debate.
"Understanding the dynamics of these immune cells is essential for elucidating asthma mechanisms and developing targeted therapies," explains Dr Samhita.
Biologic drugs like monoclonal antibodies (e.g., dupilumab, mepolizumab, and omalizumab) have been designed to block key cytokines such as IL-5 and IL-13. While these therapies have proven beneficial for some patients, others show limited response, indicating the presence of additional immune mechanisms that require further exploration.
"Notable controversies surrounding asthma treatment include the efficacy of biologic therapies aimed at modulating type 2 inflammation and the implications of emerging immune cell populations identified as potential contributors to asthma exacerbations."
Research suggests that novel immune cell subtypes may influence the severity of asthma symptoms. This revelation is pushing scientists to reconsider existing treatment strategies and investigate alternative approaches for severe asthma cases that are resistant to conventional therapies.
Also read: From Allergies to Asthma, These Conditions Can Trigger Nasal Polyps
The Impact of Genetics on Asthma Development

Genetics also plays a significant role in determining an individual’s susceptibility to asthma. Genome-wide association studies (GWAS) have identified specific genetic markers linked to asthma risk. "Research has identified that genetic predispositions play a significant role in asthma development," says Dr Samhita.
Some key genetic factors associated with asthma include:
Protocadherin-1 (PCDH1) – Implicated in airway epithelial barrier function, which affects sensitivity to allergens.
Cadherin-related family member-3 (CDHR3) – Linked to severe childhood asthma, particularly in cases triggered by viral infections.
Orosomucoid-like protein isoform-3 (ORMDL3) – Regulates inflammatory pathways in the lungs, contributing to asthma severity.
These genetic variations influence how the immune system responds to environmental triggers, reinforcing the need for personalised treatment strategies.
The Future of Asthma Treatment
Personalised medicine is emerging as the future of asthma management. Understanding individual immune cell activity, genetic predispositions, and environmental influences will allow for tailored therapies that improve patient outcomes. "The interplay between genetic predispositions and environmental triggers, such as allergens and respiratory infections, shapes individual immune responses in asthma," Dr Samhita explains.
With ongoing research, scientists aim to refine treatment approaches, enhance early diagnosis, and develop novel interventions that address asthma at its root cause rather than merely managing symptoms.
Conclusion
Asthma is more than just an allergic response; it is a complex condition driven by immune cells and genetic factors. By continuing to study the immune mechanisms behind asthma, researchers hope to develop more effective, personalised treatments that will significantly improve the quality of life for millions affected by this chronic disease.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version
