
Tularemia, widely recognized as "rabbit fever," has shown a dramatic surge in human cases across the United States over the past decade, according to a recent Centers for Disease Control and Prevention (CDC) report. While rare, this serious bacterial infection caused by Francisella tularensis poses significant health risks, with a variety of transmission routes contributing to its spread.
Table of Content:-
What Is Tularemia?
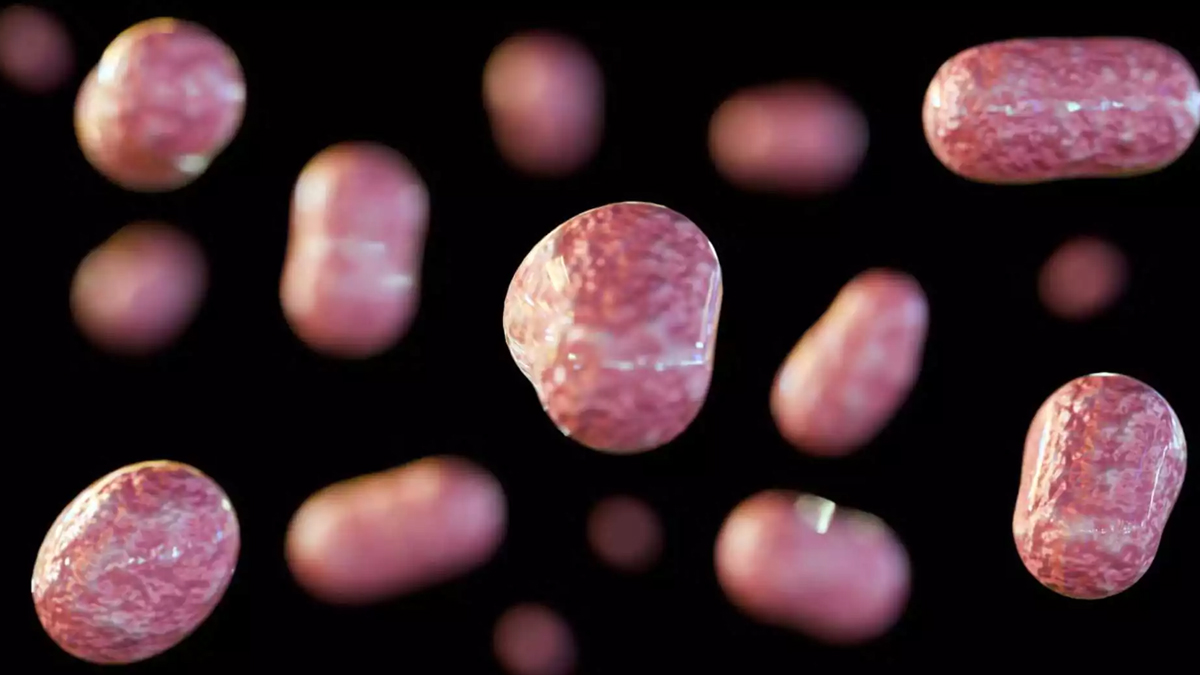
Tularemia primarily impacts wildlife, especially rabbits, hares, and rodents. Humans can contract the disease through multiple exposure routes, including:
- Insect Bites: Ticks and deer flies are common carriers of the bacteria.
- Direct Contact: Handling infected animals or their tissues can lead to transmission.
- Aerosolized Bacteria: Activities like mowing over contaminated nests can release the bacteria into the air, causing inhalation-related infections.

One notable example of aerosolized transmission occurred in Massachusetts in 2000, when lawn mowing at a vineyard caused 15 cases and one fatality in just six months. Similarly, outbreaks in Colorado in 2014 and 2015 highlighted the risks of accidental exposure through such activities.
Rising Cases and Improved Detection
Between 2011 and 2022, the CDC recorded 2,462 tularemia cases across 47 states—a 56% increase compared to the previous decade. Although the disease remains rare, affecting approximately one person per 200,000 annually, the upward trend is concerning.
Also Read: Malaysia on Alert as HMPV Cases Spike Following China Outbreak: Prevention Tips You Need to Know!
Advancements in diagnostic technology have likely contributed to this increase in reported cases. In 2017, the CDC updated its criteria for "probable cases" to include those detected via polymerase chain reaction (PCR) testing, boosting the accuracy and frequency of diagnoses. Of the reported cases:
- Confirmed Cases: 984 were confirmed through bacterial isolation or significant antibody changes.
- Probable Cases: 1,475 were classified as probable, accounting for 60% of total cases—an increase from the 35% seen in the previous decade.
Challenges in Diagnosing and Treating Tularemia
Tularemia's symptoms can vary based on how the infection is contracted, making diagnosis a challenge. Common symptoms include:
- Fever and chills
- Fatigue and body aches
- Localized pain or swelling
Also Read: Are We Heading for Another Pandemic? Highly Infectious Diseases to Watch in 2025
Left untreated, tularemia can lead to severe complications, and in some cases, death. The CDC reports that the overall fatality rate is typically below 2%, though certain strains and conditions may elevate this risk. Prompt diagnosis and treatment with antibiotics are essential for managing the disease effectively.
Preventive Measures to Reduce Risk
Preventing tularemia requires awareness of its transmission modes and adopting measures to minimize exposure. Here are some practical tips:
Protect Against Insect Bites
- Use insect repellents containing DEET.
- Wear long sleeves and pants when outdoors.
- Perform tick checks after spending time in wooded or grassy areas.
Handle Wildlife Safely
- Avoid direct contact with sick or dead animals.
- Use gloves when handling animal carcasses.
Mow with Caution
- Check the area for signs of wildlife nests before mowing.
- Avoid mowing over potentially contaminated zones.
Maintain Hygiene
- Wash hands thoroughly after outdoor activities or handling animals.
- Ensure proper food handling to avoid contamination.
Bottomline
Although tularemia remains a rare disease, its growing prevalence highlights the importance of education, preventive practices, and early medical intervention. With continued improvements in diagnostic techniques and awareness campaigns, the risk of serious complications from rabbit fever can be significantly reduced.
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version