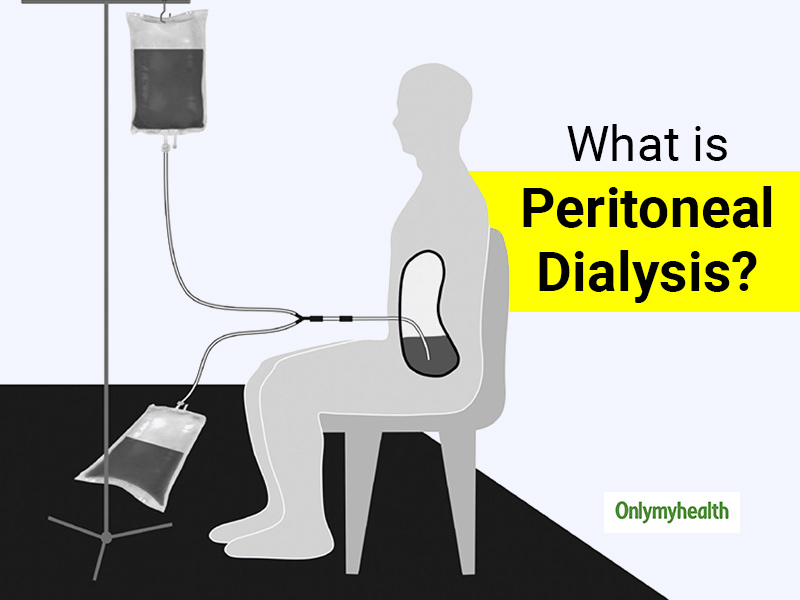
What is Peritoneal Dialysis? When your kidneys can no longer adequately remove waste products from your blood, then the procedure of peritoneal dialysis is used. PD or peritoneal dialysis is a therapy that uses peritoneum (a natural membrane lining inside the abdominal cavity) as a biological filter. It also has similar attributes to the artificial filter, which is used in haemodialysis. While retaining others, its pores allow the passage of certain substances. Due to poor hygiene, contaminated equipment or unclean surroundings, an infection may occur during peritoneal dialysis. How is the need for peritoneal dialysis diagnosed? It is often diagnosed by analyzing a sample of the infected fluid taken from the belly (abdomen). Other tests for peritonitis may include X-rays. Imaging tests take pictures of your body's tissues, bones, and organs. Medical scientists have devised a technique that would make peritoneal (a large part of the stomach) dialysis much easier. It has a wearable artificial kidney, which works on its own. During peritoneal dialysis, this artificial kidney is very useful in removing toxins from the patient's blood. It has been claimed in a recent study.
Table of Content:-
Common causes of ruptures that lead to peritoneal dialysis include:

- Peritonitis: It may develop as the use of feeding tubes, a procedure to withdraw fluid from your abdomen, the complication of gastrointestinal surgery, and rarely as a complication of endoscopy or colonoscopy. Common symptoms behind peritonitis are: bloating in your stomach with a feeling of fullness, loss of appetite and low urine output, tenderness or abdominal pain, inability to pass gas or stool. fever, fatigue, diarrhoea and vomiting or nausea.
- A stomach ulcer, perforated colon or ruptured appendix: Any of these situations can allow bacteria to get through a hole into the peritoneum (in your gastrointestinal tract).
- Pancreatitis: It is also known as the inflammation of your pancreas. Also, when the bacteria spread outside the pancreas may lead to peritonitis.
- Diverticulitis: Infection of bulging, small pouches in your digestive tract may cause peritonitis if one of the pouches ruptures, spilling intestinal waste into your abdominal cavity.
- Trauma: Trauma or injury may cause peritonitis by allowing chemicals or bacteria from other parts of your body to enter the peritoneum.
Also Read: Food’s Impact on Diabetes: These 2 Diet Concepts Are Sure To Help In Diabetes Management
Peritoneal Dialysis: When Should One Seek Medical Advice?
Dialysis is needed when the kidney stops functioning. Peritoneal dialysis involves placing liquids in the patient's abdominal cavity through a unique plastic tube to remove excess waste products and fluid from the body. It uses body tissue to act as a filter. If you are receiving peritoneal dialysis, contact your health care provider immediately if your dialysis fluid:
- Is cloudy or has an unusual colour
- Contains white flecks
- Contains strands or clumps (fibrin)
- Has an unusual odour, especially if the area around your tube (catheter) is red or painful.
Also Read: End-Stage Renal Disease On Peritoneal Dialysis: What Is The Reason Behind Death In Patients?
How to manage the side effects of peritoneal dialysis?
Routine tests should be scheduled. This also involves taking samples of drained fluid and blood, which is then sent to a lab. The outcomes will determine how well peritoneal dialysis is removing wastes from the bloodstream. Based on these results, the treating nephrologist may make changes, to ensure dialysis prescription provides good removal of excess fluid and waste from the body to ensure the best dialysis and quality of life.

What are the medications for peritoneal dialysis?
Medications for peritoneal dialysis include:
- Erythropoietin: Nearly all patients with (ESRD) end-stage renal disease who are on dialysis, have anaemia. Hence, erythropoietin is a medication that one is prescribed
- Iron
- Active Vitamin D
- Phosphorus binders
- B-complex Vitamin and folic acid
- Topical creams and antihistamines
- Vitamin E
Also Read: Dialysis During Pandemic? Here Are Some Responsible Steps Patients Must Take
What are the risk factors for peritoneal dialysis?
Risk factors of peritoneal dialysis could include:
- Infections: Peritonitis, i.e. infection of the abdominal lining is a usual complexity of peritoneal dialysis. An infection can also develop where the catheter is inserted (at the site) to carry the dialysate (cleansing fluid) out of your abdomen. The risk of contamination is higher if the person doing the dialysis is not adequately trained.
- Weight gain: The dialysate includes dextrose (sugar). Absorbing some of the dialysates might cause you to take extra calories (in hundreds) daily, leading to additional weight gain. The extra calories can also cause diabetes, especially if you have high blood sugar.
- Inadequate dialysis: Do you know that peritoneal dialysis can become ineffective after several years? You might need to switch to hemodialysis.
- Hernia: Holding fluid in your abdomen for extended periods may strain your muscles.
Also Read: Some Tips To Control The Occurrence Of Diabetes In Dialysis Patients

PERITONEAL DIALYSIS: Here are some points to remember
If you have peritoneal dialysis, you will need to avoid:
- Over-the-counter medications and specific prescription which can damage your kidneys include nonsteroidal anti-inflammatory drugs.
- Soaking in a hot tub or bath, swimming in a pond, lake, river or nonchlorinated pool increases infection risk. Swimming or taking in a chlorinated pool is generally acceptable.
- Protocols to decrease infection risk in PD or peritoneal dialysis patients include proper catheter placement, exit-site care that provides for Staphylococcus aureus prophylaxis, thorough training of patients with periodic retraining, treatment of contamination, and prevention of procedure-related and fungal peritonitis.
Also Read: Dr Raman Tanwar Explains The Link Between Diabetes and Kidney Stones
FAQs related to peritoneal dialysis
- What is the connection between diabetes and peritoneal dialysis? Since PD or peritoneal dialysis uses glucose (sugar-based solutions) to perform dialysis, people with diabetes starting peritoneal dialysis often see a rise in their blood sugar levels. Sugar levels greater than 300 mg/dl, i.e. (very high levels) can occur in peritoneal dialysis patients, but it is uncommon to cause symptoms.
- How does it feel to be living with peritoneal dialysis? Unless the patient is very sick for reasons other than kidney failure, dialysis should help them feel better. Some people feel better for the first week. Others notice a difference after a few months. If the dialysis treatments make you feel ill or tired, one should tell their primary care professional about the symptoms to help them feel better.
- Is there any self-treatment for peritoneal dialysis? Evidence suggests that promoting self-management improves the health status of peritoneal dialysis (PD) patients. After a set period, the fluid with the filtered waste products flows out of your abdomen and is discarded. These treatments can be done at work, home or while travelling.

- Do medications cause fatal Peritonitis? There have concerns about the effectiveness of once-daily intraperitoneal dosing of cephalosporins in patients on peritoneal dialysis (PD), and recommendations including antibiotics in each bag of dialysate for patients on automated PD or converting to continuous ambulatory PD for the duration of therapy. However, this is quite cumbersome for patients dialyzing at home.
- Is peritoneal dialysis possible with an artificial kidney? The research study was presented at the ASN Kidney Week held at the Walter E. Washington Convention Center in the US capital, Washington DC. Researchers have been investigating this device's potential, called the Automatic Wearable Artificial Kidney (AWAK), to be useful in peritoneal dialysis. The results of this technique are encouraging during testing. If this technology is finally successful, it will revolutionize peritoneal dialysis. This will significantly reduce the time it takes for dialysis and relieves the hassle of hours of pre-dialysis therapy and the need to connect larger machines. Through this, the patient will also be able to do dialysis by himself.
(With inputs from Dr Salil Jain, Nephrologist, Fortis Gurugram)
Read More Articles in Other Diseases
Also watch this video
How we keep this article up to date:
We work with experts and keep a close eye on the latest in health and wellness. Whenever there is a new research or helpful information, we update our articles with accurate and useful advice.
Current Version